In addition to making an estimated 5,830 Kenai Peninsula residents eligible for Medicaid, the Medicaid expansion being debated in the Alaska Legislature could have behind-the-scenes effects on a health care system currently dealing with 9,239 unprocessed applications.
The 2010 Affordable Care Act gives state governments incentives to offer Medicaid to individuals earning below 138 percent of the Federal Poverty level — for Alaska residents, an annual income of less than $20,313. Yet even without expansion, the ACA has already impacted local Medicaid providers and administrators through its online health care marketplace.
Peninsula Central Health Service Outreach, PCHS, and Affordable Care Act, ACA, Enrollment Coordinator Tina Wegener, who has been helping PCHS users enroll in ACA care, said the marketplace website was designed to channel eligible applicants into Medicaid.
“When people apply for marketplace insurance, if it looks like they would qualify for Medicaid, then (the marketplace software) does kind of stop them and say ‘please apply for Medicaid,’ Wegener said. “The computer system is set up where it says ‘send the information to the state.’”
At the state level, the information is evaluated by the Department of Health and Social Services’ Division of Public Assistance, DPA, which handles Medicaid enrollment. The enrollment application ultimately ends up on the desk of someone like Kirk Roesing, director of the DPA’s Eligibility Office in Kenai.
Roesing said the number of people brought into Medicaid through the ACA had a noticeable impact on his office.
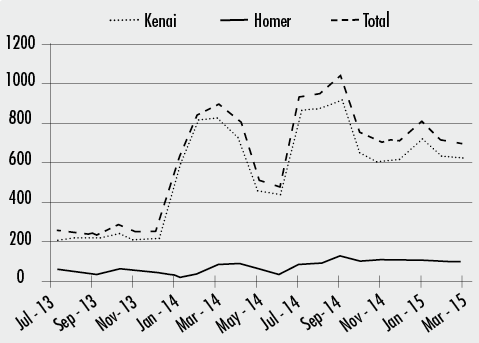
“January 2014 is when things really started to happen,” Roesing said. “We went from approximately 200 or so Medicaid applications in this office a month up to — in January it went up to 576, then in February to 800. … It hasn’t really gone down since then.”
These numbers may not overburden the Kenai office, since applications received in a particular DPA eligibility office are not necessarily processed in that office.
In order to distribute the workload, Roesing said that online Medicaid applications received by DPA “go into a pool, and are distributed on a random basis” among offices throughout the state.
However, the increased number of Kenai applicants have contributed to the growing statewide backlog of unprocessed Medicaid applications. As of April 6, 2015, 9,239 Medicaid applications had been held without an eligibility determination for longer than 90 days, an increase from 6,325 undecided applications in December 2014.
“We’re not coping with it as well as I’d hope we could,” Roesing said. “Even if we were able to add positions, it takes a while to get people up to speed. But we were not really able to add positions until recently. We were able to add some temporary positions to help cope with it. They’re in the training process and getting up to speed right now.”
In an email by Alaska Department of Health and Social Services Public Information Officer Catherine Stadem, members of the DHSS Medicaid Expansion Team stated that the department has 363 staff members working overtime to alleviate the backlog.
The Division of Public Assistance is also in the process of phasing out its current software, the 31-year-old Eligibility Information System, and replacing it with Alaska’s Resource for Integrated Eligibility Services (ARIES), a web-based system capable of better interfacing with the health care marketplace software. The ARIES project, begun in 2012, was financed with $65 million in federal funds.
If Medicaid is expanded, the federal government will cover 100 percent of the estimated $145.4 million annual care expenses until 2017, when Alaska will begin contributing a 5 percent annual share, to be to raised to a permanent 10 percent share by 2020. Stadem wrote that this federal money “will pay for medical care services provided directly to participants in the program in health clinics, pharmacies, hospitals and doctors’ offices across the state.”
Stadem wrote that the federal Medicaid program will also pay for half the estimated $2 million administration costs. In the first year of expansion, the other half will be paid by the Alaska Mental Health Trust Authority, and thereafter from the state general fund.